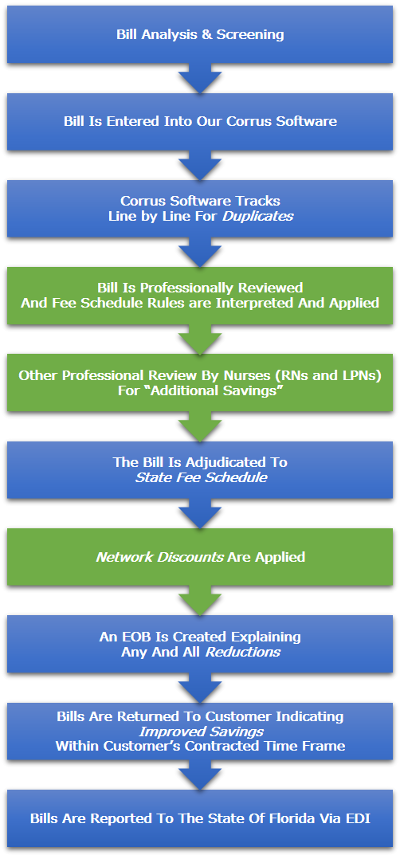
Automated bill review plays a major part in managing workers' compensation medical costs. Medical bill review is a cost containment tool that can show hard dollar reductions. Soft savings may be realized by the identification of case management opportunities and reduced administrative costs. AmeriSys has trained analysts; professional nurses and/or physician advisors review provider bills.
Medical Fee Schedules A statutory medical fee schedule sets a maximum amount that a medical provider is reimbursed for rendering medical services to a person injured at work. Our system adjudicates the medical provider's charges to those allowed under the statutory medical fee schedule and is equipped with a rules engine that assists in navigating the complexities of limits and rules in bill review. Additionally, the accuracy of the CPT codes, unbundling and the level of service are verified. The diagnosis is checked for relatedness to the reported injury and all applicable claims information is reported to the Division as required.
Provider Network(s) AmeriSys has a one step process that allows for the PPO reduction to be applied to the mandatory fee schedule or the usual and customary amount. AmeriSys has the ability to utilize multiple PPO networks/or can accommodate custom networks, payment modules, or negotiated rates on an individual clinician level.
Ancillary Services AmeriSys has partnered with industry leaders instrumental in providing services required for timely and cost effective claims handling. These services include Durable Medical Equipment, Diagnostic services, transportation and translation as well as Home Health, Rehabilitation and Physical Therapy. In addition these providers have electronic billing capabilities directly to the AmeriSys system for timely process of medical billings.
Claim History AmeriSys collects the historical data from the injured employee's reviewed medical bills. This 'history' provides a record of the medical treatment rendered and makes it easy to identify the employee's medical providers and their treatment patterns.
Duplicate Billings Duplicates are identified to the bill review staff in two ways. Exact duplicates which match all criteria including same FEIN, date of service, coding and billed amount.
Possible duplicates are also identified which would alert the reviewer to a previously paid bill that only has the same coding and date of service. We find this is particularly important as provider services are often billed under a separate FEIN when a billing service is utilized, or multiple providers are attempting to bill for the same service such as diagnostic interpretation. The notification of "possible duplication" would allow the reviewer to question the charges thoroughly prior to reimbursement.
Medical PEER Review (complex bill review) AmeriSys submits provider bills to qualified physician advisors when there is a questions of medical necessity, over-utilization of services, length of stay determination, patterns of practice determinations or to determine proper bill coding. AmeriSys matches the provider specialty when choosing a physician to review a provider bill.
Turn Around Time The normal turn around time for provider bills received is 72 hours once the bills are received in our office. If additional information is needed the turn around time may be lengthened until information is received.
Explanation of Bill Review (EOBR) Each bill adjudicated is returned with an EOBR that identifies the reductions and the recommended reimbursement allowance.
Reports AmeriSys produces reports from the automated bill system. These reports include but are not limited to Savings Reports, Outcome Reports, and Network Hits Reports.
Interface It may be possible to interface with your claims system for transfer of provider bill information to include the billed charges and the recommended reductions.
Invoicing AmeriSys has the capability to utilize an aggregate invoice for provider bill services while providing a detailed report of the individual bills for your review.